Effects of Radiation Treatment on Wound Healing
Radiation therapy is often necessary to treat cancer and can be very effective. It uses high-energy particles or waves such as x-rays, gamma rays, electron beams or protons to destroy or damage cancer cells. Unfortunately, radiation treatment can also injure blood vessels that transport the oxygen needed for tissue healing. As a result, cancer survivors are at higher risk of developing non-healing wounds, even up to 20 years after treatment. Specialized wound care can help.
There are two common types of radiation injuries.
1. Osteoradionecrosis (ORN) is bone injury caused by radiation that often occurs to the jaw bone or mandible.
- Often arises after tooth extraction in patients with prior radiation therapy.
- Patients can experience pain, difficulty opening the mouth, exposed and or damaged bone, drainage and swelling.
2. Soft Tissue Radionecrosis (STRN) is damage to skin, muscle or organs caused by radiation
- Although any tissue may be affected, STRN is found often in the head, neck, chest, breast and pelvis
- It can be broken down into external and more internal injuries.
- External injury is most often seen in the form of non-healing wounds in areas of the body that had previously been treated with radiation.
- Common examples of internal injury are radiation cystitis and radiation proctitis and are due to radiation treatment in the abdomen or groin region.
- Radiation Cystitis is damage to the bladder.
- Common symptoms include urinary urgency, pain and incontinence.
- Look out for blood in the urine, inflammation of exposed areas, pain and open, non-healing wounds.
- Radiation-induced Proctitis is damage to the rectum.
- Symptoms include diarrhea, rectal urgency and rectal bleeding.
- Additional risk factors include infection, prior ischemia, immunodeficiency, diabetes, steroid use, anti-rejection medications in transplant patients, and the size and location of the tumor.
Depending on the type of injury, a patient may receive hyperbaric oxygen therapy (HBOT) alone or as part of a comprehensive wound care plan. Hyperbaric oxygen therapy improves healing and prevents breakdown of tissue exposed to radiation by increasing the amount of oxygen in the blood. During the treatments, the patient breathes 100 percent oxygen inside a pressurized chamber, quickly increasing the concentration of oxygen in the bloodstream, where it is delivered to a patient's wound site for faster healing. Patients who are currently receiving chemotherapy must have a thorough review by a hyperbaric physician before being treated for injuries since some drugs may have adverse effects. Medicare covers hyperbaric oxygen therapy for several types of chronic wounds.
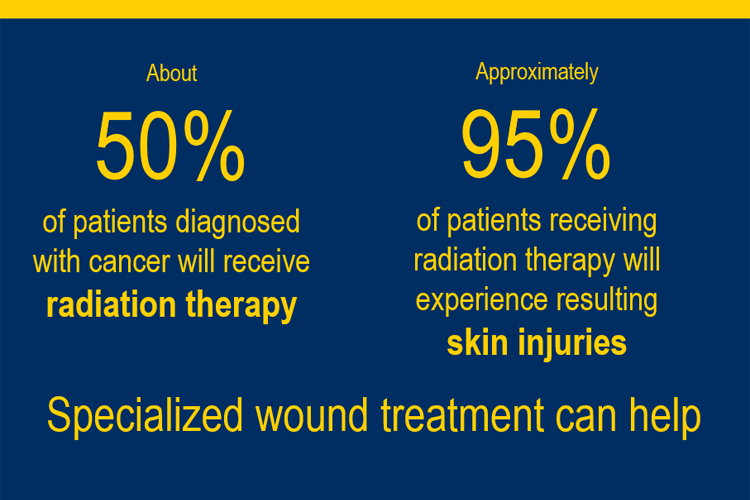
Roughly half of patients diagnosed with cancer are prescribed radiation therapy, and many will experience skin injuries as a result. If you are experiencing a non-healing wound or any of the symptoms described here, talk to your doctor and/or seek out a specialized Wound Treatment Center.
Travis Taylor, D.O., is the medical director of the Wound Treatment Centers in Gladwin and Alpena, and co-director of the Wound Treatment Center in Midland. He specializes in Emergency Medicine, Hyperbaric Medicine and Wound Treatment.